Ultrasound of parotid gland
Anatomy of Parotid Glands
The parotid glands are the largest salivary glands. They are located just in front of the ears. The saliva produced in these glands is secreted into the mouth from a duct near the upper second molar tooth.
Each parotid gland has two parts, or lobes: the superficial lobe and the deep lobe. Between the two lobes is the facial nerve. The facial nerve is important because it controls our ability to close our eyes, raise our eyebrows, and smile.
Other critical structures near the parotid glands include the external carotid artery, which is a major supplier of blood to the head and neck region, and the retromandibular vein, a branch of the jugular vein.
In the parotid gland, unlike the submandibular and sublingual glands, lymph nodes may be found.
In about 20% of the population, an accessory parotid gland may be present, being located superficially to the masseter muscle with drainage through the parotid duct. This can also be a location of benign or malignant parotid tumors and should therefore be searched for.
Imaging:
The glands are best visualized with a high frequency transducer (10-15MHz) with assessment in two perpendicular planes. In addition, a curvilinear lower frequency (5-10MHz) can be used to assess the deep aspect of the parotid gland.
Pathology:
- INFLAMMATORY AND INFECTIOUS DISORDERS:
- ACUTE INFLAMMATION:
In children, the main cause is viral parotitis (usually caused by mumps).
Glands become enlarged and hypoechoic. They may be heterogeneous, with oval and small hypoechoic areas, representing secretions foci. They may have increased blood flow and reactive lymph nodes may be present.
In cases of bacterial etiology, the inflammation can be complicated by abscess.
At US, these lesions are hypoechoic or anechoic with posterior acoustic enhancement and unclear borders and may be surrounded by a hyperechoic “halo”. There can be an avascular area with debris (central liquefaction) and gas (hyperechoic foci).
- CHRONIC INFLAMMATION
Chronic recurrent parotitis may cause relapsing episodes of inflammatory parotid enlargement. Its etiology is unknown, but some proposed causes include recurrent infections or autoimmune diseases.
US demonstrates normal sized or smaller parotid, hypoechoic or inhomogeneous (tiny anechoic spaces, due to sialectasis, and small round hypoechoic nodes, representing secretions and intraparotid lymph nodes). Usually there is not an increased vascularization. Calcifications are better seen on CT.
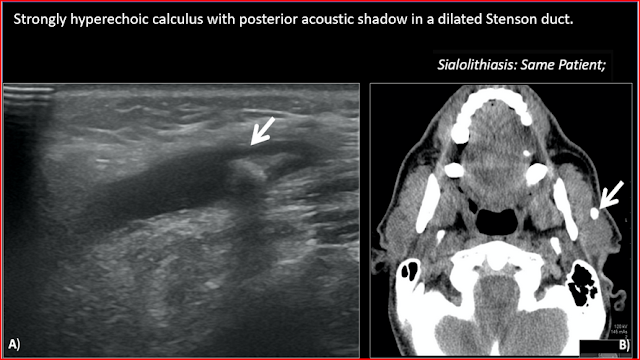
- SIALOLITHIASIS:
The clinical history is usually of recurrent pain and swelling of the affected gland, particularly related to meals.
US is an important tool as a first-line assessment of ductal ectasia and lithiasis. Besides calculi, imaging may show associated features, such as ductal ectasia, heterogeneous gland parenchyma and possible abscesses. It is important to determinate the location of the stone (intraductal or intraglandular). However, small calculi (inferior to 2-3 mm) may not be detected. CT provides a good detection of calculi and assessment of adjacent gland.
- SYSTEMIC DISORDERS:
It is a noninflammatory and non-neoplastic condition of non tender chronic enlargement of the parotid glands, affecting less commonly the other glands. It is usually bilateral and symmetric.
- NEOPLASMS
Regarding salivary glands, the rate of malignancy decreases as the size of the gland increases. It's not easy to differentiate the several types of tumors that involve the parotid gland because they share clinical and imaging features. On imaging, features that suggest malignity include ill-defined margins with invasion of other cervical planes and cervical lymphadenopathy.
The treatment of choice for benign and malignant parotid tumors is partial or total parotidectomy, according to the extent of the tumor.
BENIGN NEOPLASMS
About 80% of parotid tumors are benign.
- CYSTS
The patients are usually asymptomatic.
Cysts can be divided into salivary duct cysts (retention cyst), lymphoepithelial cysts (branchial cleft cyst), HIV-associated parotid disease (lymphoepithelial sialadenitis), dermoid cysts and lymphangioma.
In terms of radiologic differential diagnosis, a cystic lesion with a well-defined margin and no solid component is usually a helpful MRI finding.
- PLEOMORPHIC ADENOMA (PA):
PA is the most common benign parotid gland tumor, occurring most often in middle-aged women, in the fourth and fifth decades of life. It presents typically as a solitary, slow-growing and painless mass.
Several patients show malignant transformation (carcinoma ex pleomorphic adenoma).
US demonstrates a lobulated and well-defined hypoechoic mass with associated posterior acoustic enhancement. On Doppler, vascularization is often absent. On CT, when small, they have homogeneous attenuation and prominent enhancement. When larger, they can be heterogeneous with less prominent enhancement, foci of necrosis, and possible delayed enhancement. Small regions of calcification are common.
-WARTHIN TUMOR (WT):
Warthin tumor is a benign neoplasm that does only occur in the parotid gland. It is the second most common tumour of the parotid gland and typically presents as a painless and slow growing mass. It is more common in men, in their 5th and 6th decades of life. The association with smoking has been proven.
WT rarely shows malignant transformation.
On US, most tumors tend to be ovoid and hypoechoic masses with well-defined margins, which may be partially or completely cystic (sponge-like anechoic areas). These tumors are often hypervascularized.
-HEMANGIOMA:
It is more frequent in the first year of life, usually with spontaneous regression in adolescence. On US, a homogeneous and lobulated hypoechogenic mass with very high internal vascularization is observed.
-LIPOMA:
Lipoma often arises in the context of trauma. These are compressible, oval and hypoechoic lesions with sharp margins and hyperechoic linear structures distributed within the lesion (striated pattern). Usually, no flow signs are detected with color Doppler examination.
MALIGNANT NEOPLASMS
Unlike benign salivary neoplasms, malignant tumors may grow rapidly, may be tender or painful at palpation, may be fixed to the background and cause facial nerve paresis or paralysis.
- MUCOEPIDERMOID CARCINOMA:
Mucoepidermoid carcinoma is the most common malignant tumor found in the parotid gland. It is more common in adults, between 30 and 50 years of age, typically presenting as a slow-growing mass.
On US, it shows typically as a well-circumscribed hypoechoic lesion, with a partial or completely cystic appearance. The lesion stands out against the relatively hyperechoic normal parotid gland.
On CT, low-grade tumors appear as well-circumscribed masses, usually with cystic components. The solid components enhance and calcification is sometimes seen. High-grade tumors on the other hand, have poorly defined margins, infiltrate locally and appear solid.
-ADENOID CYSTIC CARCINOMA:
It's the second most common malignancy involving the parotid gland. They are locally aggressive with a propensity for perineural spread, which is well appreciated on MRI.
On CT, generally, a distinction is made radiologically between low-grade and high-grade adenoid cystic carcinomas. Low-grade tumors tend to be well-defined, in contradiction to high-grade tumors, which appear infiltrative. However, both subtypes are usually homogeneously enhancing after contrast administration.
- OTHER PRIMARY MALIGNANT NEOPLASMS are rare and the different forms of primary malignancy are not readily differentiated using ultrasound.
- LYMPHOMA:
Primary and secondary lymphoma of the parotid are rare. Patients with Sjögren's disease, HIV and chronic sialadenitis are at higher risk of parotid lymphoma. US shows several or a solitary hypoechoic lesion, which may present internal septa. A focal or diffuse involvement of the gland may be seen, along with enlarged intraparotid lymph nodes.
- METASTASES:
Primary tumors metastasizing to salivary glands may be located in the head and neck region, as well as in more distant parts of the body. Melanoma, spinocellular cancer, breast cancer, and lung cancer may produce metastases to intraparotid lymph nodes.
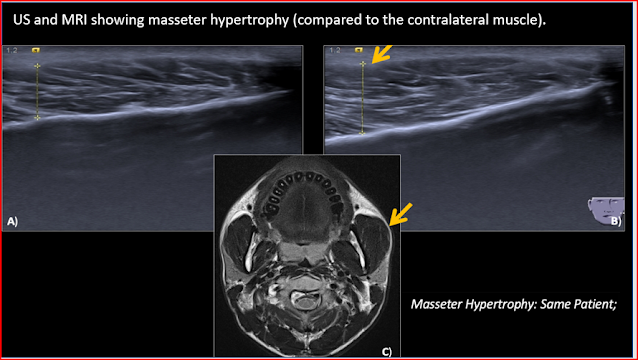
- CONDITIONS THAT MIMIC PAROTID ENLARGEMENT
One condition that may mimic a parotid enlargement is masseter hypertrophy. This can be seen on MRI, as an enlarged masseter with normal signal intensity.





















0 Comments